The Human Impact of Leading-Edge Science
Medical Breakthroughs
Modern medical science keeps bringing us closer to treatments and cures we need to live a healthy life — reversing disease-causing genetic mutations by altering DNA, removing and replacing vital organs and rebuilding neurological connections in the brain.
To most of us, such advances are just jargon, but six local residents know first-hand how medical science miraculously relieves human suffering. Their stories illustrate the impact of recent medical breakthroughs on real people living in our community.
Two New Lungs – Danny Sam
In January 2023, Lake County resident Danny Sam received a double lung transplant, a medical procedure he considers a miracle. That’s not surprising considering that a matched donor became available when he needed two new lungs.
A double lung transplant sounds like some space-age medical miracle, but the surgery has been around for the last three decades.
“The actual miracle is not the procedure itself but the fact that we’ve improved the technique to make transplant a viable option for a broader range of patients,” explains Dr. Amir Emtiazjoo, UF Health Shands Lung Transplant Program medical director.
The procedure is actually quite similar to a single lung transplant performed twice. The patient is put on a machine that temporarily breathes for him while the surgeons remove and replace each lung, one at a time.
According to Dr. Emtiazjoo, a key element to a successful lung transplant is having a team that works together harmoniously and effectively with the patient to make the miracle happen.
Approximately 74 U.S. hospitals can perform a double lung transplant with varying levels of expertise.
“It’s about the expertise of the whole hospital, from the pre-care coordination to surgery to intensive care recovery and carrying on to post-care coordination,” explains Jamie Burrows, BSN, CCRN-K, UF Health Shands Lung Transplant Program manager.
The operation is the crucial part, but patient selection and post-operative care are important for the best outcome.
“You need the whole orchestra, not just the piano,” Dr. Emtiazjoo says.
Lung transplant programs like the one at UF Health Shands can offer a higher level of expertise because they handle a larger volume and more complex cases, which allows staff to improve their skills.
“At UF Health Shands, we do between 50 and 100 lung transplants a year compared to some other programs that only do 10 or 20,” Jamie says.
There are several conditions a patient must meet. First and foremost: a willingness to exercise regularly and make healthy dietary changes.
A prospective lung transplant patient might be disqualified if he or she is an active smoker, is severely debilitated or does not have a strong care provider plan for support throughout the process and follow-up.
On March 1, 2023, Danny walked out of UF Health Shands under his own power with his new lungs, forever grateful for the transplant team and for the medical breakthrough of a double lung transplant.
To learn more about the lung transplant program at UF Health Shands, visit their website: https://ufhealth.org/conditions-and-treatments/lung-transplant.

Remission Without Chemo – Bob Tracey
You probably think of chemotherapy when you hear about cancer treatment. That was Bob Tracey’s first thought when he was diagnosed with chronic lymphocytic leukemia (CLL) in 2017. His second thought was an image burned into his brain of his father-in-law, a thin, pale, almost ghost-like version of himself trying to survive chemo and beat cancer.
When Bob was diagnosed with CLL, his doctor tried to soften the news by telling him and his wife, Ann, that the disease was no big deal, that they could control the disease and Bob would be fine.
Bob wasn’t buying it.
“I looked at Ann and asked what her father died of, although I already knew,” Bob says.
In front of the doctor, in that tense moment, Ann articulated Bob’s concerns. When her father received his diagnosis, the doctors said it was no big deal, but he died a year later after an agonizing attempt at treatment.
For Bob, immunotherapy was the medical breakthrough that kept him from repeating his father-in-law’s fate.
CLL, the most common form of leukemia in adults, is a blood cancer that begins in the bone marrow. Immunotherapy has replaced chemotherapy as the most effective treatment for blood cancers such as CLL.
“Bob didn’t get chemotherapy—the stuff that makes you lose your hair,” explains Dr. Maen Hussein, oncologist at Florida Cancer Specialists. “Oncology is evolving very fast. We’re having much better outcomes and far fewer side effects with immunotherapies.”
The chemotherapy used to treat CLL was highly toxic when Ann’s father was diagnosed 20 years ago. It killed cancer cells, but it was mostly indiscriminate, killing all kinds of cells, good and bad. Many patients did not survive the side effects of the high doses needed to attack blood cancers.
Immunotherapies, like the treatment Bob had, stimulate the immune system to fight the cancer. They can target and block specific proteins the cancer cells require to grow and multiply, thereby stopping the cancer from taking over and crowding out healthy cells.
Using the immune system to fight cancer is an idea first explored at the end of the 19th century. The discovery of T cells in the 1960s pushed the idea further toward today’s reality of a viable treatment option.

Stopping the Tremors of Parkinson’s – Jane Masterson
In January, the Food and Drug Administration (FDA) approved the latest version deep brain stimulation (DBS) device for Parkinson’s. Although DBS is not a new treatment, recent improvements to the device bring added convenience to people living with Parkinson’s, along with more information-gathering capacity for medical scientists still looking for a cure for the disease.
And although Parkinson’s comes with a wide range of symptoms, tremors may be one of the most common.
People living with Parkinson’s, like Jane Masterson of The Villages, often develop tremors that keep them from performing daily activities like signing their name, writing a grocery list, pouring a cup of tea, feeding themselves and managing their own self-care.
Jane was diagnosed with Parkinson’s in 1997 and had her first DBS implant in 2010 to control significant tremors on the left side of her body.
“Like magic, the tremors went away,” says Jane, co-author of the book Our Parkinson’s Disease Instruction Manual. A year later, she had another DBS implant in the left side of her brain to manage right-side tremors.
Jane refers to her two brain surgeries as if they were no big deal. In fact, each implant required surgeons to shave her head and cut into her skull to insert an electrode in just the right spot.
“My head healed, and my hair grew back. It was important to me to stop the tremors so I could be more independent again,” Jane explains.
The DBS device sits beneath the skin just below the collarbone and is attached by fine wires that run under the skin to the electrode deep inside her brain.
But brain surgery was not the end of the process. Programming began once Jane recovered from surgery. A neurology technician adjusted the DBS controller and Jane went home to see how they worked. There were several trips back and forth to get the individual settings right and maintain optimal functioning.
After 10 years of managing her tremors, Jane’s initial DBS device was turned off because it developed a defect that would require surgery to repair. Unfortunately, replacing the DBS wasn’t an option.
Fourteen years after her first brain surgery, Jane’s health has declined and anesthesia is no longer an option.
Jane still benefits from her other DBS, which can be reprogrammed to keep up with her changing condition.
“That’s one of the hallmarks of this disease is that it’s always changing,” Jane explains. “You might control the symptoms for a time, but they will be back and other symptoms will develop.”
Jane knew the day would come. It does for everyone living with Parkinson’s.
“My suggestion to anyone considering DBS for Parkinson’s is to not wait until your tremors are severe because eventually you will no longer be a candidate for surgery,” Jane shares.
Jane may be out of options today, but tomorrow could bring the next breakthrough. Medical science is always changing in an effort to keep up and one day get in front of neurological conditions like Parkinson’s.
The latest version of the DBS device, Medtronics Percept includes a 15-year battery that recharges in an hour. That’s a convenient upgrade from the 5-year batteries used in Jane’s devices. The Medtronics Percept, can also be programmed remotely, eliminating many trips to the medical office.
Perhaps the most promising part of this new device is the inclusion of BrainSense technology, which captures and records brain signals. Neurologists no longer have to rely on information from the patient to program the device for optimal functioning. They can use the recorded data to personalize DBS therapy.

Building New Neuropathways – John Rosenwinkel
In March, stroke survivor John Rosenwinkel traveled to Tampa General Hospital to have a device implanted just under his collarbone and wired to the side of his neck.
The Vivistim device stimulates the vagus nerve during therapy exercises to boost the brain’s neural activity and helps build new neuropathways for controlling arm and hand movement.
This medical breakthrough is a game-changer for victims of stroke, the leading cause of death in the U.S. according to the Center for Disease Control and the leading cause of disability according to the American Stroke Association.
During a stroke, the brain is damaged when blood flow is interrupted and brain cells are deprived of oxygen. Those who survive a stroke are often left with partial paralysis, an inability to speak, chronic pain, memory loss, anxiety and depression.
Depending on the extent of the damage, some abilities lost may be recovered in the first several months after the stroke. But recovery generally hits a plateau. To move past this recovery plateau, the brain needs to build new neural pathways, an ability called neuroplasticity.
John remained on that plateau for five years before learning about the new device reported to increase neuroplasticity for stroke survivors with diminished upper extremity functioning.
In John’s case, the Vivistim was activated by his physical therapist via remote control during six weeks of in-clinic rehabilitation. For at-home exercises between therapy sessions, John activated the Vivistim with a magnet.
Therapy activities are customized to the patient’s abilities and goals. Stimulating the vagus nerve while performing repetitive motions helps build neuropathways faster than regular physical therapy. Adding 30-minute sessions of home exercise further speeds improvement.
With the help of Vivistim, patients with limited arm and hand movement due to a stroke are again able to participate in daily living activities like showering, cooking meals, buttoning their shirts or playing cards.
We had a patient who wanted to mow his lawn again, and one who wanted to be able to cast his fishing rod,” says Terri Stemple, territory manager for MicroTransponder, the manufacturer of Vivistim. “We had a patient recently who could not pick up a pen, and at the end of six weeks of therapy he wrote me a birthday card and signed his name.”
In just a few months following the implant, John went from having little functionality in his right hand to cutting his own meat and clipping his fingernails by himself.
“He can even drive with his right hand and write a little, and he’s still improving,” Sue, John’s wife, explains. “All in all, we’re very happy with the device. People that haven’t seen him in a while can really see his progress.”
Ideal candidates for Vivistim Therapy are ischemic stroke survivors with chronic upper limb motor deficiencies who are healthy enough for surgery and have enough motor control to participate in physical therapy. For more information, go to vivistim.com.
Avoiding Clots and Excessive Bleeding – Steve Negen
Steve Negen is using the latest version of the Watchman to get off the blood thinners he’s taken for the last 15 years. Living without that medication will open a whole new world of possibilities for Steve.
The Watchman, a permanent implant designed to close the left atrial appendage in the heart, was originally approved by the Food and Drug Administration (FDA) in 2015 as an alternative to blood thinners for reducing the risk of stroke.
Steve’s heart troubles began in 2009 when he survived a heart attack likely brought on by an allergic reaction to medication he received during a stent procedure. Ten years later, he had a stroke a couple months after neck surgery.
Stroke victims are often prescribed blood thinners because they keep blood cells from sticking together and forming clots that can cause heart attack, stroke, or pulmonary embolism.
But blood thinners have their drawbacks. One of the more serious side effects of blood thinners is excessive bleeding because the blood doesn’t clot easily. That can make medical procedures risky.
“Every time I have a procedure, like my colonoscopy next week, I have to stop taking the blood thinners for four days,” Steve says. “There’s no telling what could happen in those four days.”
Blood clots often form in that left atrial appendage, a small side compartment of the heart. By closing off this compartment, the Watchman prevents clots from forming.
The latest version of the Watchman, the Watchman FLX, includes upgrades like a new polymer coating that reduces the risk of blood clots forming around the device and enables faster healing from the procedure. New markers on the device make it easier to see and implant in exactly the right location. The Watchman FLX is also available in a wider range of sizes that allow the right fit for more patients.
“The biggest improvement in this latest version Watchman is in the safety profile,” says Dr. Gregory O. von Mering, who performed the Watchman procedure at HCA Florida Heart and Lung in Ocala. “The new coating on the outside of the device facilitates the growth of tissue over the device without risk of forming clots.”
Steve is understandably anxious about another heart attack or stroke since he’s experienced both and therefore may be at a higher risk of developing a blood clot. Since his stroke, Steve is not steady on his feet, making him a fall risk. Any time he bumps into something, Steve bruises right away.
“The Watchman is essential to patients like Steve who don’t tolerate blood thinners well. Before the Watchman came along, there was no alternative treatment,” Dr. von Mering explains.
Steve is looking forward to putting the risk and cost of blood thinners behind him. And as he looks forward, beyond the Watchman, he is hopeful to be a candidate for Vivistim so he can continue his stroke recovery.

Delivering Dopamine for the Brain – Bill McKinney
If you ask Pokhui McKinney to name the most significant medical breakthrough of this decade, she’ll tell you about the Duopa that allowed her husband to walk again.
Pokhui knew something was wrong when she noticed her husband Bill walking without moving his left arm. Bill, a career military man who had spent a couple years in Vietnam and was exposed to Agent Orange, was diagnosed with Parkinson’s in 2008.
Ten years later, Bill was retired from the military and working a civilian job when his tremors got so bad that he could not stand still to make the presentations his job required. He had to resign. In 2020, a bout of COVID accelerated Bill’s Parkinson’s symptoms and he could no longer walk.
The medication could not keep up with Bill’s accelerated symptoms, as often happens in advanced Parkinson’s. Bill was taking 18 pills a day at extremely high doses, but his tremors were not under control.
“With the tremors on his left side, and dragging his left leg, Bill had some spectacular falls, on planes, in church. He fell in the washroom and broke his right femur neck,” Pokhui explains.
Today, Bill no longer takes any pills for Parkinson’s, and he walks without a walker or a cane. The difference is Duopa.
Duopa is a delivery system for Parkinson’s medications that bypasses the digestive system and goes directly into the small intestine. Duopa, which is administered in gel form every three to four seconds consistently throughout the day, provides better results than pills that are broken down in the stomach and absorbed into the blood stream at varying rates.
A PEG-J tube implanted in Bill’s abdomen provides a direct line to his intestine. The tube runs externally to a pump that is programmed for his specific needs. The medication is contained in a cassette that is plugged into the pump.
Bill was admitted to the hospital for the PEG-J tube, though it is usually done as an outpatient procedure. Dr. Robert Hawes from Orlando Health Endoscopy made sure Bill’s tube was positioned correctly.
On July 16, Bill went to the Parkinson’s Foundation Center of Excellence in the Fixel Institute in Gainesville to have the Duopa pump attached to the J-tube and programmed. Results came almost immediately.
“Bill could barely walk with his walker, but when we came back from lunch he was walking on his own,” Pokhui said.
Exercise and routine are the two most important elements to slowing the symptoms of Parkinson’s. Bill and Pokhui have a new morning routine with Doupa.
“I get up at 5:30 every morning and take a cassette out of the refrigerator to warm up. At 6, I connect the room temperature cassette to Bill’s pump,” Pokhui explains. “It takes about a minute. He’s usually still sleeping.”
Exercise is better for Bill now that he can walk without assistance. He still shuffles a little, but he is much steadier on his feet than he used to be. Bill participates in the Power with Parkinson’s Fitness program at Genesis Health Club, where boxing is used for physical and mental fitness.
“I boxed when I was at West Point; I was regimental champion,” Bill says. “It’s great to be able to box again, at least in the gym.”
Bill and Pokhui know three other people who have the Duopa, and Bill’s results are more dramatic than theirs.
“Doupa is a miracle for Bill,” Pokhui exclaims.
Duopa is approved for people with Parkinson’s who experience three hours or more of “off” time, when their tremors are not well-controlled, each day.
Focus on Alzheimer’s
Nearly seven million Americans are living with Alzheimer’s, a disease that kills more than breast cancer and prostate cancer combined, according to the Alzheimer’s Association. Recent medical breakthroughs could help reduce the number of new cases and speed up diagnosis.
Lowering Risk
A study recently concluded that people who eat at least two servings a week of processed red meat have a 14% higher risk of developing Alzheimer’s or other forms of dementia than those who eat no more than three servings a month.
The massive study, reported at the Alzheimer’s Association International Conference in July, followed more than 130,000 people for up to 43 years. Participants who ate bacon, hot dogs, kielbasa, salami, bologna and other processed red meats were more likely to develop dementia.
“Processed red meat has also been shown to raise the risk of cancer, heart disease and diabetes. It may affect the brain because it has high levels of harmful substances such as nitrates (preservatives) and sodium,” says Yuhan Li, MHS, lead author of the study.
Researchers also concluded that replacing a daily serving of processed red meat with a serving of non-meat protein source like nuts, beans or tofu, every day could reduce the risk of developing dementia by 20%.
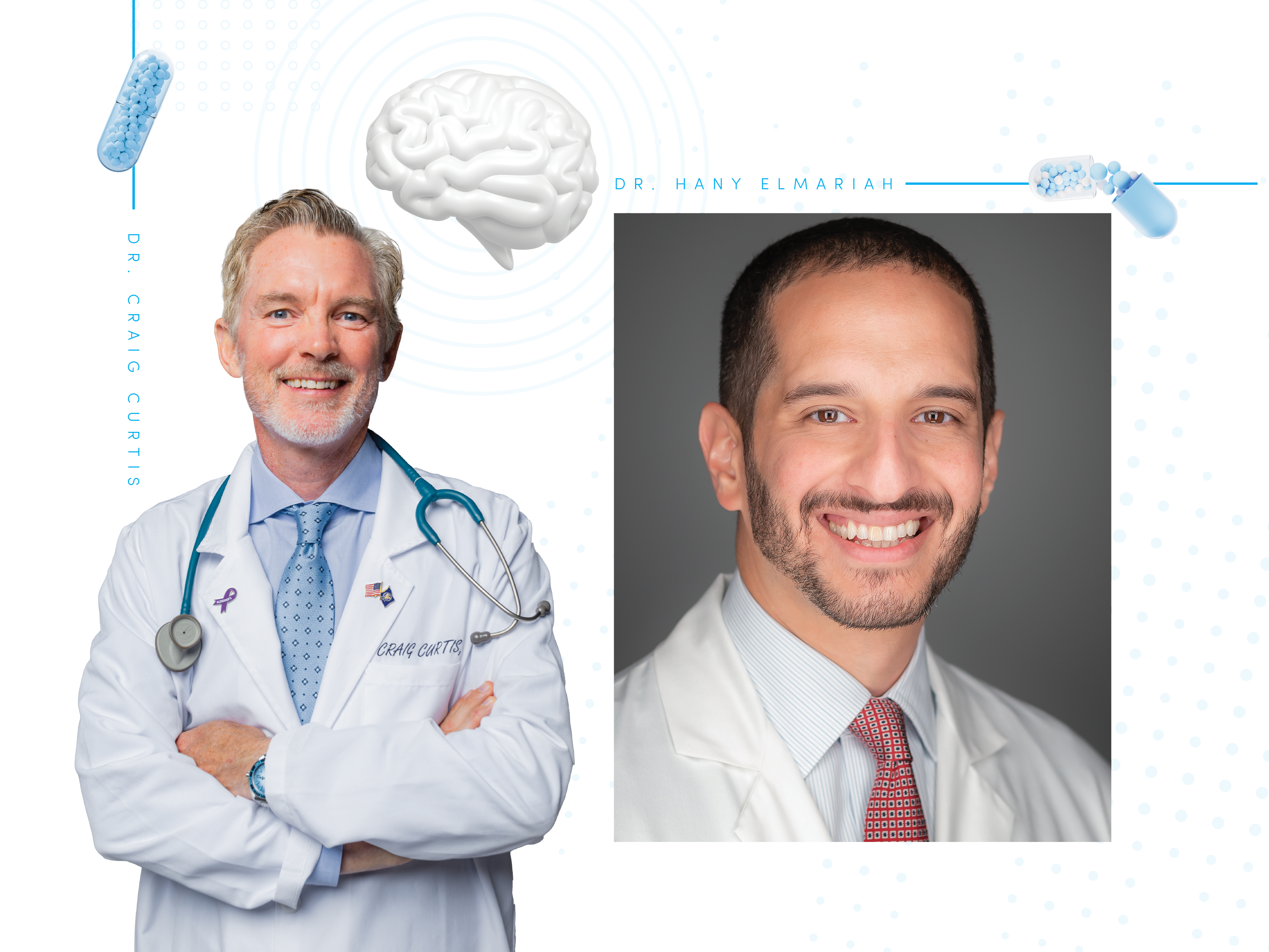
“Science is showing there are many lifestyle changes we can make to lessen our risk of Alzheimer’s, and this latest finding identifies another change you can start today,” says Craig Curtis, MD, founder of K2 Medical Research.
Reducing Diagnostic Time
A blood test exhibited high diagnostic accuracy for detecting Alzheimer’s, according to a study published in the Journal of the American Medical Association at the end of July. The ability to diagnose Alzheimer’s with a blood test could speed up the diagnostic process and alleviate long wait times to see specialists.
People are becoming more aware of the early signs of Alzheimer’s and overwhelming neurologists for appointments to begin the lengthy evaluation process. A blood test that can be administered by primary care physicians could help triage the flood of patients seeking evaluation and assuage the fears of many with mild cognitive issues not related to Alzheimer’s.
“Only a small portion of patients who get in to see a memory specialist need to be there. This new diagnostic tool can empower primary care physicians to make informed decisions about the need for specialist appointments,” Dr. Curtis says.
Gene Therapy for Blood Cell Mutations
The Food and Drug Administration (FDA) have approved the first cell-based gene therapies for sickle cell disease, a medical breakthrough that represents the first real chance for a cure for many people living with this life-threatening blood disease.
“Historically, allogeneic bone marrow transplant was the only potential cure. While this treatment is effective, it requires the use of bone marrow from a compatible donor,” says Dr. Hany Elmariah, an associate member of the Blood and Marrow Transplant and Cellular Immunotherapy at Moffitt Cancer Center.
Sickle cell, the most commonly inherited blood disease, affects about 100,000 Americans according to the Center for Disease Control (CDC), a majority of whom are African American.
The disease is a protein mutation in red blood cells which limits oxygen delivery to the tissues, causing severe pain and organ damage and limiting life expectancy by up to 20 years.
“New gene therapies attack the underlying cause of sickle cell by reprogramming the patient’s own bone marrow so that it stops making sickle cells and starts making normal blood. Since it uses the patient’s own marrow, this treatment is feasible even for patients who do not have a compatible donor,” Dr. Elmariah explains.
Two newly-approved treatments — Casgevy and Lyfgenia — focus on altering stem cells and returning them to the body. Stem cells collected from the patient are genetically modified and then returned via infusion to stimulate the production of healthy red blood cells.
“It is still early to know how gene therapy will work in the real world. But the early studies have shown incredible results that will be life changing for our patients and hopefully paradigm shifting for how we treat sickle cell and other similar blood diseases,” Dr. Elmariah concludes.

