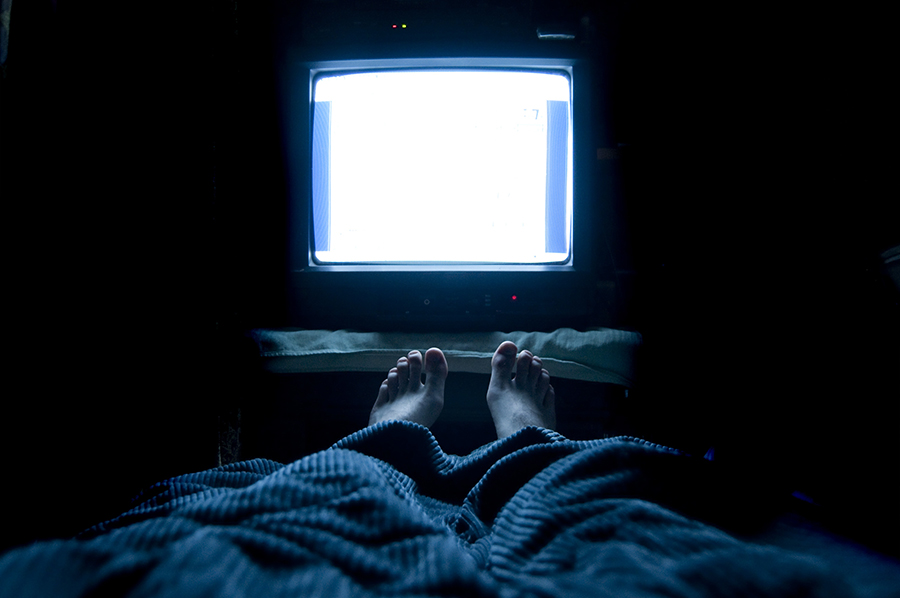
Restless legs and your sleep
A neurological condition that makes sleep difficult, restless legs is a disruptive disorder.
Story: Dr. Alex Dimitriu
The cause of an individual case of insomnia may be as elusive as the sleep so hard to come by. It can be associated with a wide range of underlying medical and psychological conditions. Anxiety comes with being unable to sleep. But sometimes insomnia isn’t caused by anxiety or medication or any of the other possible culprits. Sometimes it is a consequence of restless legs syndrome, a condition so disruptive to restful sleep that it is considered a sleep disorder.
Restless legs syndrome (RLS), also known as Willis-Ekbom disorder, is a common neurological condition that causes unpleasant sensations in the legs or other parts of the body and an irresistible urge to move the legs to relieve the sensations. Patients may find it difficult to describe these sensations, using words such as itching, throbbing, pins and needles, or a “creepy-crawly” feeling. These sensations are worse when sitting or lying down and tend to be more severe late in the day and at night, which impairs getting restful sleep.
It is estimated that 7 percent to 10 percent of the U.S. population suffers from RLS. It affects both genders but is more common in women, and while it can start at any age, those most severely affected are middle-aged and older.
The cause of RLS isn’t known, but it tends to run in families and iron deficiency may play a role. Some cases are associated with an underlying condition, such as Parkinson’s disease, kidney failure, or peripheral neuropathy, but most often, there is no other condition. Certain medications, including anti-depressants like SSRIs, as well as mood stabilizers can result or worsen RLS and the insomnia it causes.
Patients with known or existing RLS should discuss this with their health-care provider. Dopamine-blocking mood stabilizers or antipsychotics for bipolar disorder, can make RLS worse and, in some cases, temporarily spread up the body creating a condition known as akathisia, often called “RLS of the whole body.”
There is no test that can confirm a diagnosis of RLS, but tests are used to rule out other conditions.
There is no cure for RLS. If there is an underlying condition, treating that condition may relieve symptoms. But for primary RLS treatment is targeted to managing the disorder, minimizing symptoms, and improving sleep. It may include the following:
Lifestyle changes: Eliminating or reducing the use of alcohol and tobacco, establishing regular sleep habits, moderate exercise, leg massage, and hot baths or heating pads may relieve symptoms.
Iron supplements: For people with low or low-normal levels of iron, iron supplements may help.
Medications: There is no single medication for RLS that works for everyone and it may be necessary to try several before choosing one. Among the choices are dopamine-related drugs like those used to treat Parkinson’s disease, although long-term use may make symptoms worse; opioids, which carry the risk of addiction but are effective for some people in low doses; and benzodiazepines, generally prescribed for anxiety, can help RLS sufferers get restful sleep.
RLS afflicts sufferers twice: first with the symptoms of the condition itself and then with chronic sleep disruption and its ill effects. While research is ongoing to identify specific changes in the brain that cause the disorder, careful management and conscientious adherence to prescribed therapies can minimize the effects of RLS.
About the writer
Dr. Alex Dimitriu is double board-certified in psychiatry and sleep medicine and is the founder of the Menlo Park Psychiatry and Sleep Medicine Center in California. See doctoralex.com.